Document Type : Original article
Subjects
Abstract
Background: The aim of the study was to determine the anatomical variations of the sphenoid sinus and its adjacent critical structures using Cone-Beam Computed Tomography (CBCT).
Methods: This cross-sectional study was conducted on CBCT scans of 67 females and 84 males between 18 to 67 years. Presence/absence of intersphenoid septa, sphenoid sinus pneumatization and its type (conchal, presellar, sellar, and postsellar a and b), protrusion of the optic canal and carotid canal into the sphenoid sinus, optic canal and carotid canal dehiscence, and Anterior Clinoid Process (ACP) pneumatization was evaluated on CBCT scans, and their prevalence and correlation were calculated. Data were analyzed by the Chi-square test (alpha=0.05).
Results: The prevalence of intersphenoid septa was 98.68%. Postsellar type a was the most common type of sphenoid sinus pneumatization with a prevalence of 41.3%. The prevalence of conchal, presellar, sellar and postsellar b types was 0, 11, 30, and 17.7%, respectively. The prevalence of optic canal and carotid canal protrusion into the sphenoid sinus was 50 and 52.7%, respectively. The prevalence of optic canal and carotid canal dehiscence was 48.3 and 40.3%, respectively. The prevalence of ACP pneumatization was 45%. Optic canal and carotid canal protrusion had a significant correlation with ACP pneumatization (p<0.001). Also, carotid canal and optic canal protrusion and dehiscence were significantly correlated with degree of sphenoid sinus pneumatization (p<0.001).
Conclusion: Sphenoid sinus pneumatization significantly increases the likelihood of carotid canal, optic canal protrusion into the sphenoid sinus and their dehiscence, therefore, a preoperative 3D imaging is strongly recommended prior to trans-sphenoidal surgical procedures.
Keywords: Carotid artery, Optic nerve, Prevalence, Septa
Introduction
Among the paranasal sinuses, the sphenoid sinus is the most inaccessible, which is surrounded by important critical anatomical structures such as the internal carotid artery and the optic nerve (1,2). The paranasal sinuses are air-filled cavities surrounded by skull bones, and are divided into anterior and posterior paranasal sinuses. The sphenoid sinus and the posterior ethmoid sinus comprise the posterior paranasal sinuses. The right and left sphenoid sinuses are often asymmetrical, and separated from each other by a thin bony septum. They are radiographically detectable from 4 years of age (1-3). The sphenoid sinus has the highest frequency of anatomical variations among different sinuses in the human body. The degree of pneumatization of the sphenoid sinus is determined based on the location of posterior sinus wall relative to sella turcica. The sphenoid sinus can have different degrees of pneumatization, ranging from no pneumatization to extensive pneumatization. In the latter case, the bone covering the carotid artery, optic nerve, and nerve of the pterygoid canal (Vidian nerve) may be thin or even non-existent, making these vital structures susceptible to iatrogenic trauma (4).
At present, endoscopic surgery of the sphenoid sinus is an acceptable technique for treatment of sinus problems and adenomas of the pituitary gland, and serves as an alternative to trans-cranial surgery, which is highly invasive and is associated with high rates of complications, morbidity and mortality (2,4-6). However, all surgical approaches (trans-ethmoidal, trans-nasal, and trans-septal) access sella through the sphenoid sinus in microscopic or endoscopic surgical procedures (4,6,7), and therefore, are associated with high risk of injury to the internal carotid artery and uncontrolled bleeding, which would often result in indirect damage to the optic nerve due to poor visibility (8,9). Thus, sufficient knowledge about the anatomical variations of the sphenoid sinus and its adjacent vital structures can substantially lower the risk of postoperative complications (8-10). Also, safe access to the pituitary gland is affected by the pneumatization pattern of the sphenoid sinus. Moreover, anatomical variations of the sphenoid sinus can predispose it to recurrent or chronic sinusitis (11,12). Despite the significance of this topic, it has not been adequately addressed in the Iranian population. Thus, the aim of the study was to determine the anatomical variations of the sphenoid sinus and its adjacent critical structures in an Iranian population using Cone-Beam Computed Tomography (CBCT).
Materials and Methods
This cross-sectional study was conducted on maxillary CBCT scans of 151 patients (300 sphenoid sinuses) retrieved from the archives of the Radiology Department of School of Dentistry, Shahid Beheshti University of Medical Sciences (ethical approval code: IR.SBMU.DRC.REC.1399.077). All CBCT scans had been taken with NewTom VGi CBCT scanner with 12×8 cm field of view between September 2019 to August 2020 for diagnostic purposes not related to this study, such as temporomandibular problems, impacted teeth, or implant treatment.
The inclusion criteria were maxillary CBCT scans of males and females over 18 years of age, that visualized the sphenoid sinuses.
The exclusion criteria were distorted images with scattered radiation or severe beam hardening artifacts, and CBCT scans with evidence of trauma, previous sphenoid sinus surgery, or sinonasal tumors.
The sample size was calculated to be a minimum of 300 CBCT scans considering the mean prevalence of optic canal and carotid canal protrusion and Anterior Clinoid Process (ACP) pneumatization to be 26.5%, and d=0.05.
The retrieved eligible CBCT scans were evaluated with OnDemand 3D version 1 software to assess the prevalence of intersphenoid septa, sphenoid sinus pneumatization and its types (conchal, presellar, sellar, and postsellar a and b), protrusion of the optic canal and carotid canal into the sphenoid sinus, optic canal and carotid canal dehiscence, and ACP pneumatization in axial, sagittal, and coronal planes.
Intersphenoid septa: Presence/absence of inter-sphenoid septa was evaluated on coronal sections. Intersphenoid septum was defined as a skeletal septum that divides the sphenoid sinus into at least two separate cavities (Figure 1).
Sphenoid sinus pneumatization type
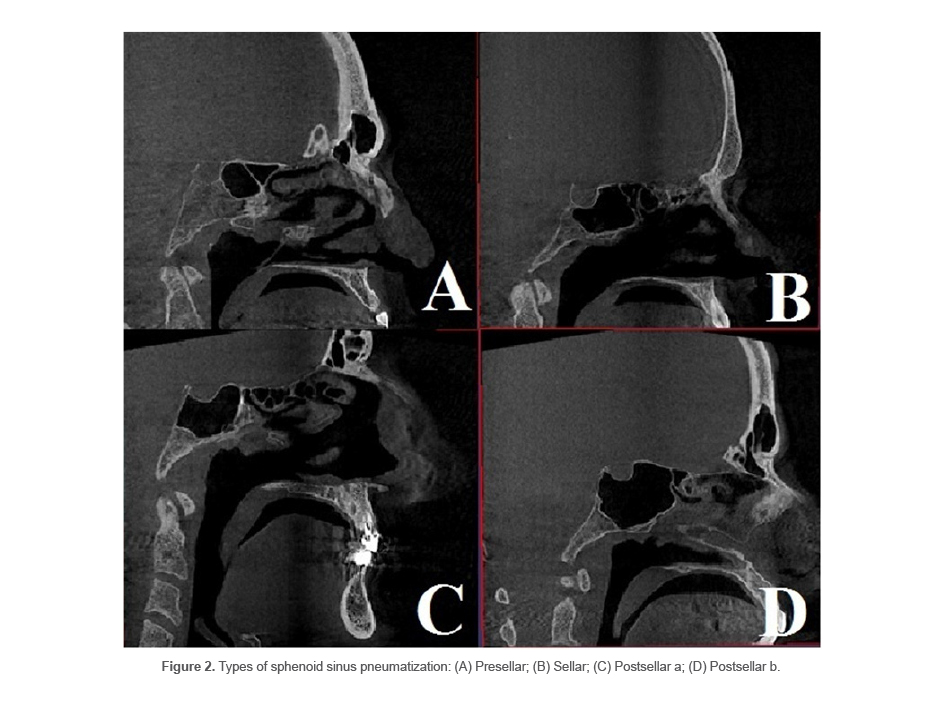
The type of pneumatization of the sphenoid sinus is determined based on the correlation of sphenoid sinus with sella turcica in the sagittal plane, which is categorized into four main types. To outline the sella turcica, two vertical lines were drawn from the most prominent anterior and posterior points of sella turcica. The four main types are as follows:
Type 1 or conchal type: Absence of sinus or very small extension of the sinus (Figure 2A).
Type 2 or presellar: The posterior wall of the sphenoid sinus is located in front of the anterior wall of sella turcica (Figure 2B).
Type 3 or sellar: The sinus is located between the anterior and posterior walls of sella turcica (Figure 2C).
Type 4 or postsellar: The posterior sinus wall exceeds the posterior border of sella turcica. Type 4 has two subtypes of a and b. In subtype a (Figure 2D), sinus pneumatization does not include the posterior clinoid process. In subtype b (Figure 2F), sinus pneumatization is so extensive that includes the posterior clinoid process (13).
Protrusion of optic canal and carotid canal into the sphenoid sinus
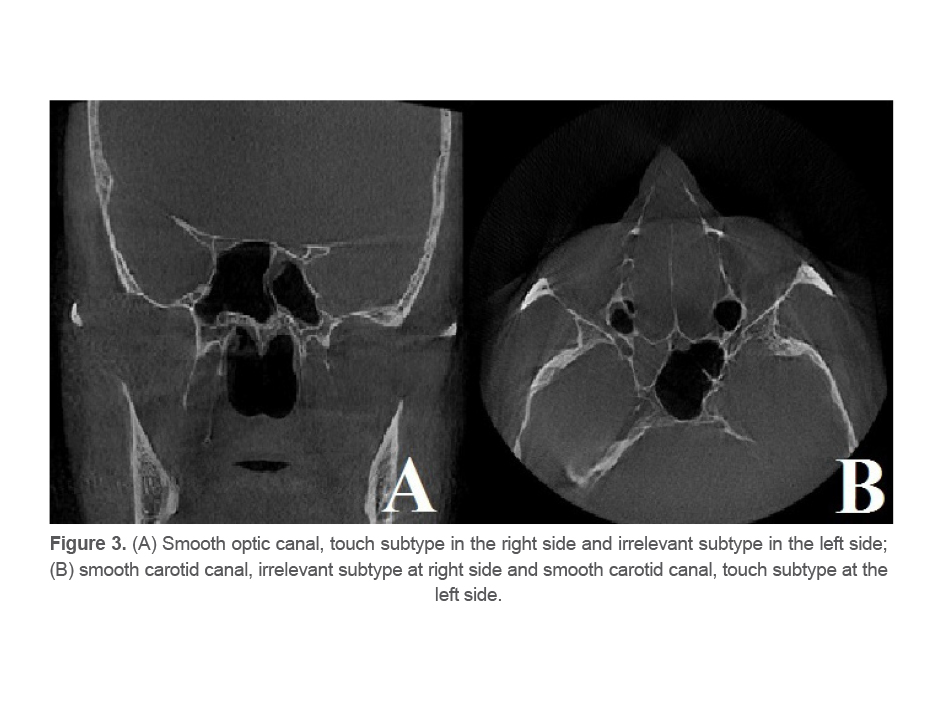
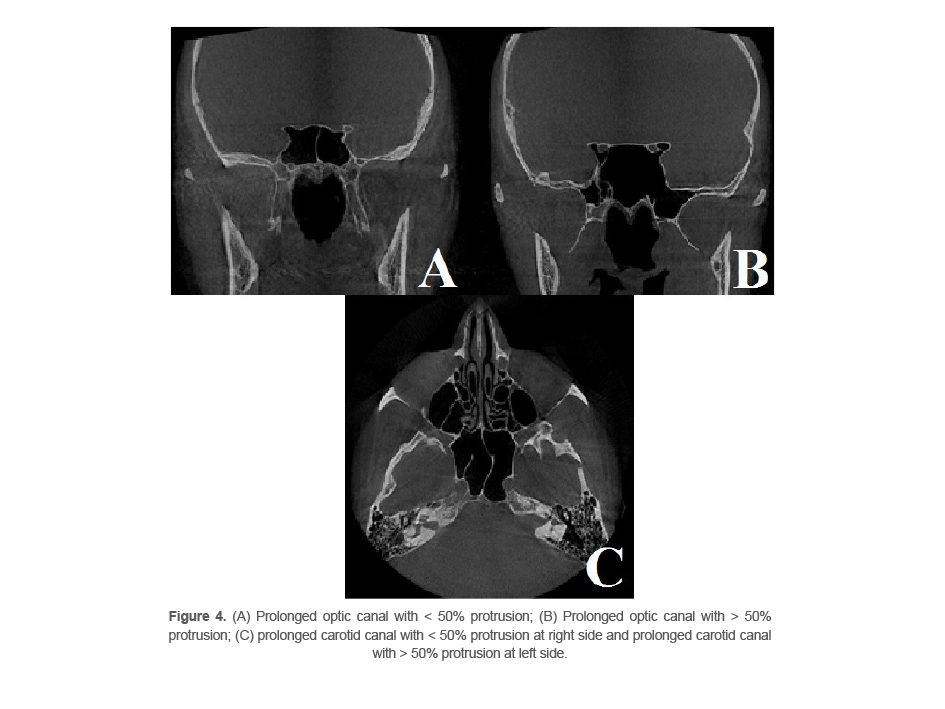
Protrusion of carotid and optic canals into the sphenoid sinus was evaluated on axial and coronal sections. Two main types have been defined in this respect as follows:
Smooth: No protrusion of optic canal or carotid canal into the sinus cavity is seen. In fact, the canal and sinus cavity either have no close correlation, which is referred to as “irrelevant” subtype, or, they have a close correlation and are attached to each other with no protrusion, and no sign of these canals exists in the sinus; this form is referred to as the “touch” subtype (Figure 3).
Prolonged: Protrusion of canals into the sphenoid sinus is evident, and depending on the degree of protrusion, it can be categorized as <50% or >50% subtype (4) (Figure 4).
Dehiscence of optic and carotid canals
In the coronal plane, dehiscence of optic canal was detected as fading of part of the opaque rim around the optic nerve (Figure 5).
In the axial plane, dehiscence of carotid canal was detected as fading of part of the opaque rim around the internal carotid artery (Figure 5).
Pneumatization of ACP
ACP pneumatization was detected as extension of the sphenoid sinus into the ACP through the optic strut or anterior root in the coronal plane (14) (Figure 6).
To assess the reliability of the measurements, two independent researchers evaluated 20 randomly selected CBCT scans. After interobserver calibration, 20 CBCT scans were evaluated again by the main examiner after a 2-week interval to calculate intraobserver reliability.
Statistical analysis
Data were analyzed by SPSS software version 26. The Kappa coefficient was calculated to assess the inter- and intra-observer agreements. Comparisons were made by the Fisher’s exact test. Level of significance was set at 0.05.
Results
The results of inter-and intra-observer agreements
The kappa coefficient was calculated to be 0.8, thus, the reliability of the inter-and intra-observer for the measurements was confirmed.
Demographic assessments
Of a total of 300 sphenoid sinuses evaluated on 151 CBCT scans, 167 (55.7%) belonged to males (n=84) and 133 (44.3%) belonged to females (n=67). The mean age of the participants was 38.96 years (range 18 to 67 years). The mean age was 38.32 years in males, and 33.23 years in females.
Sphenoid sinus assessment
Intersphenoid septa
Intersphenoid septa was absent in 2 cases (1.32%, one male and one female), resulting in formation of one sinus cavity.
Type of pneumatization of the sphenoid sinus
Postsellar a (4a) was the most frequent type (41.3%; n=124) followed by sellar (3) type (30%;n=90), postsellar b (4b) type (17.7%; n=53) and presellar (2) type (11%; n=33). No conchal type was noted.
Protrusion of optic canal
Protrusion of optic canal into the sphenoid sinus was noted in 50% of patients; out of which, 22.7% (n=68) had over 50% protrusion, and 27.3% (n=82) had < 50% protrusion. The touch subtype (43%,n=129) had the highest prevalence, and the prevalence of irrelevant subtype was 7% (n=21).
Protrusion of carotid canal
Protrusion of carotid canal was seen in 52.7% of patients; out of which, 19.3% (n=58) had protrusion > 50%, and 33.3% (n=100) had protrusion <50%. The frequency of touch and irrelevant subtypes was 25% (n=75) and 22.3% (n=67), respectively.
Dehiscence of optic canal
Optic canal and carotid canal dehiscence were recorded in 48.3% (n=145) and 40.3% (n=121) of the patients, respectively.
ACP pneumatization
ACP pneumatization was noted in 45% (n=135) of the patients.
Correlation of ACP pneumatization with optic canal protrusion
The Chi-square test showed a significant correlation between ACP pneumatization and optic canal protrusion (p<0.001, Table 1).
Correlation of ACP pneumatization with carotid canal protrusion
The Chi-square test showed a significant correlation between ACP pneumatization and carotid canal protrusion (p<0.001, Table 1).
Correlation of sphenoid sinus pneumatization with optic canal protrusion
The Chi-square test indicated a significant correlation between sphenoid sinus pneumatization and optic canal protrusion (p<0.001,Table2), such that the likelihood of optic canal protrusion increased with greater pneumatization and higher type of sphenoid sinus pneumatization.
Correlation of sphenoid sinus pneumatization with carotid canal protrusion
The Chi-square test demonstrated a significant correlation between sphenoid sinus pneumatization and carotid canal protrusion (p<0.001,Table2), such that the likelihood of carotid canal protrusion increased with greater pneumatization and higher type of sphenoid sinus pneumatization.
Table 1. Protrusion of optic canal and carotid canal based on presence/absence of ACP pneumatization
|
Total |
Optic canal protrusion |
|
Total |
Carotid canal protrusion |
|
|
|
|
Present |
Absent |
Present |
Absent |
||||
|
165 %100 |
25 %15.2 |
140 %84.8 |
165 %100 |
53 32.1% |
112 67.9% |
Absent |
ACP pneumatization |
|
135 %100 |
125 %92.6 |
10 %7.4 |
135 %100 |
105 %77.8 |
30 22.2% |
Present |
|
|
300 %100 |
150 50% |
150 %50 |
300 %100 |
158 %52.7 |
142 47.3% |
Total |
|
p<0.001.
Table 2. Protrusion of Optic canal and carotid canal based on type of sphenoid sinus pneumatization
|
Total |
Optic canal protrusion |
|
Total |
Carotid canal protrusion |
|
|
|
|
Present |
Absent |
Present |
Absent |
|
|
||
|
33 100% |
5 15.2% |
28 84.8% |
33 100 % |
5 15.2% |
28 84.8% |
Type 2 |
Sphenoid sinus pneumatization type |
|
90 100% |
30 33.3% |
60 66.7% |
90 100% |
22 24.4% |
68 75.6% |
Type 3
|
|
|
124 100% |
75 60.5% |
49 39.5% |
124 100% |
96 77.4% |
28 22.6% |
Type 4a
|
|
|
53 100% |
40 75.5% |
13 24.5% |
53 100% |
35 66% |
18 34% |
Type 4b |
|
|
300 100% |
150 50% |
150 50% |
300 100% |
158 52.7% |
142 47.3% |
Total |
|
(p<0.001).
Table 3. Prevalence of optic canal and carotid canal dehiscence based on type of sphenoid sinus pneumatization
|
Total |
Optic canal dehiscence |
|
Total |
Carotid canal dehiscence |
|
|
|
|
Present |
Absent |
Present |
Absent |
||||
|
33 %100 |
26 %78.8 |
7 %21.2 |
33 %100 |
29 %87.9 |
4 %12.1 |
Type 2 |
Sphenoid sinus pneumatization type |
|
90 %100 |
62 %68.9 |
28 %31.1 |
90 %100 |
69 %76.7 |
21 23.3% |
Type 3 |
|
|
124 %100 |
48 %38.7 |
76 %61.3 |
124 %100 |
61 %49.2 |
63 %50.8 |
Type 4a |
|
|
53 %100 |
19 %35.9 |
34 %64.1 |
53 %100 |
20 %37.7 |
33 %62.3 |
Type 4b |
|
|
300 100% |
155 51.7% |
145 %48.3 |
300 %100 |
179 59.7% |
121 40.3% |
Total |
|
(p<0.001).
Correlation of sphenoid sinus pneumatization with optic canal dehiscence
The Chi-square test showed a significant correlation between sphenoid sinus pneumatization and optic canal dehiscence (p<0.001,Table 3), such that the likelihood of optic canal dehiscence increased with greater pneumatization and higher type of sphenoid sinus pneumatization.
Correlation of sphenoid sinus pneumatization with carotid canal dehiscence
The Chi-square test showed a significant correlation between sphenoid sinus pneumatization and carotid canal dehiscence (p<0.001,Table3), such that the likelihood of carotid canal dehiscence increased with greater pneumatization and higher type of sphenoid sinus pneumatization.
Discussion
Adequate information regarding the anatomical variations of the sphenoid sinus and its adjacent critical structures can substantially lower the risk of postoperative complications (15-17). Thus, this study assessed the anatomical variations of the sphenoid sinus and its adjacent vital structures in an Iranian population using CBCT.CBCT was used in this study since this imaging modality provides highly accurate information regarding anatomical variations in the maxillofacial region, and has been extensively used in the literature (18-21).
The present results revealed that the prevalence of intersphenoid septa was 98.68%. This rate was 99.2% in a study by Movahhedian et al (4), 96.6% in a study by Özer et al (7), and 89.2% in a study by Hamid et al (12).
Regarding the sphenoid sinus pneumatization type, type 1 was not observed in any patient. The prevalence of types 2, 4a and 4b was 11, 33, 41.3, and 17.7%, respectively. In general, type 4 was the dominant type in our Iranian study population with a prevalence of 59%. In the study by Movahhedian et al (4) the prevalence of types 1, 2, 4, 4a, and 4b was 1, 11.5, 35.5, 38.9, and 13.1%, respectively; in general, 52% of their study population showed type 4. Similar to the present results, Rahmati et al (6) found no case of type 1, but the frequency of types 2, 3, and 4 was 1.9, 14.6, and 83.5%, respectively, in their study. They did not separately report the prevalence of types 4a and 4b. Özer et al (7) in Turkey reported the prevalence of types 1, 2, 3 and 4 to be 1.4, 8.3, 23.6, and 66.7%, respectively. Štoković et al (22) in Serbia suggested that type 3 was the dominant type. The frequency of types 1, 2, 3, and 4 was 2, 24, 41, and 33%, respectively, in their study. However, their study had a small sample size. Güldner et al (13)evaluated 580 Swedish patients, and reported that type 3 was the dominant type. The frequency of types 1, 2, 3, 4a, and 4b was 0.3, 6.6, 57.2, 17.9, and 17.9%, respectively, in their study. In general, type 1 was the rarest type in most abovementioned studies, similar to the present study. This finding is highly important since type 1 pneumatization of the sphenoid sinus is a contraindication for trans-sphenoidal surgical procedures (23). The dominant type in the present study was 4a, which was similar to the dominant type in the study by Movahhedian et al (4); this similarity is probably due to the fact that both studies were conducted on the Iranian population. The dominant type was type 3 in the European populations as discussed earlier. Thus, variations in this regard are attributed to racial differences.
The optic canal protrusion had a frequency of 50% in the present study. This rate was 40.3% in the study by Movahedian et al (4) 33% in the study by Rahmati et al [6] 31.5% in a study by Şirikci et al (24) 53% in the study by Štoković et al (22) and 59% in a study by Hewaidi et al (25). However, optic canal protrusion had a frequency of 4.1% in a study by Kazkayasi et al (26) which was much lower than the rate reported in other studies.
The carotid canal protrusion had a frequency of 52.6% in the present study. This rate had a prevalence of 50.9% in the study by Movahedian et al (4), 38.8% in the study by Rahmati et al (6) 26.1% in the study by Şirikci et al (24) 63.6% in the study by Hewaidi et al (25) and 5.2% in the study by Kazkayasi et al (26)which was much lower than the rate reported in other studies. They probably considered different criteria for protrusion of optic and carotid canals (26). In general, the values reported by Movahedian et al (4)in their study conducted in Shiraz, Iran, were closest to our findings.
In the present study, optic canal dehiscence had a prevalence of 48.3%. This rate was 40.6% in the study by Hewaidi et al (25) and 64.2% in the study by Movahedian et al (4).
Dehiscence of carotid canal was reported in 40.3% of the patients in the present study, which was exactly the same as the rate reported by Hewaidi et al (25). This value was 42.8% in the study by Movahedian et al (4).
ACP pneumatization was found in 45% of the patients in the present study. This rate was 33.1% in the study by Rahmati et al, (6) 25.5% in the study by Burulday et al, (14) 29.3% in the study by Şirikci et al (24) 15.3% in the study by Hewaidi et al (25) and 17.2% in the study by Kazkayasi et al (26). Considering the present results and those of Rahmati et al (6) it appears that the prevalence of ACP pneumatization in the Iranian population is higher than its average global prevalence. This finding is important since anterior clinoidectomy should be avoided or done with caution in populations where the frequency of ACP pneumatization (type 3) is high. Also, according to Burulday et al (14), rate of ACP pneumatization decreases with age, which is due to the process of sclerosis in older ages. Thus, presence/absence of ACP pneumatization should be precisely evaluated prior to this surgical procedure, especially in younger individuals in Iran, which apparently has a high prevalence of ACP pneumatization (14).
In the present study, ACP pneumatization had a significant correlation with optic canal protrusion, which was similar to the findings of Rahmati et al (6), Hewaidi et al (25), and Kazkayasi et al (26). Also, ACP pneumatization had a significant correlation with carotid canal protrusion in the present study, which was in agreement with the findings of Hewaidi et al (25). However, Rahamti et al (6) and Kazkayasi et al (26) did not find a significant correlation between ACP pneumatization and carotid canal protrusion. But, it should be noted that our sample size was larger than that of Rahmati et al (6).
Sphenoid sinus pneumatization was significantly correlated with optic canal dehiscence in the present study. Similarly, Movahedian et al (4) found a significant correlation between sphenoid sinus pneumatization and optic canal dehiscence, but Štoković et al (22) and Güldner et al (13) found no such correlation.
In the present study, sphenoid sinus pneumatization had a significant correlation with carotid canal dehiscence as well. Movahedian et al (4) found a significant correlation between sphenoid sinus pneumatization and carotid canal dehiscence, but Štoković et al (22) and Güldner et al (13) did not find such a correlation.
Considering the significance of the sphenoid sinus and its anatomical variations, further studies with a larger sample size are required on the sphenoid sinus and other vital anatomical landmarks in its vicinity such as the Vidian and maxillary nerves.
Conclusion
Sphenoid sinus pneumatization increases the likelihood of carotid and optic canal protrusion into the sphenoid sinus and their dehiscence. Thus, detection of extensive pneumatization of the sphenoid sinus can serve as a predictor for higher risk of iatrogenic trauma to the internal carotid artery and optic nerve.