Document Type : Original article
Abstract
Background: There has been multiple methanol poisoning outbreaks in Iran throughout the years, thus understanding patient’s socioeconomic status, the type of alcohol they consumed or the reason behind their alcohol consumption will help us to establish ways to prevent these incidences from happening. The aim of this investigation is to assess the prognosis and complications of methanol intoxication.
Methods: This cross-sectional study was carried out on patients in Tabriz Sina Hospital during 5 months. The data of the investigated patients was entered into SPSS26. Chi-Square and Logistic Regression tests were used in this analysis.
Results: From the 184 patients, 77.72% (143) recovered completely, 14.67% (27) recovered with permanent complications, and 7.61% (14) died. The most significant predictors of mortality were an increase in levels of Basal excess and creatinine and decrease in respiratory rate, systolic blood pressure and mean arterial pressure on admission and occurrence of arrhythmia. Visual symptoms on admission had protective effects against morbidity and mortality.
Conclusion: According to this study, poor outcome was associated with respiratory rate, systolic blood pressure, mean arterial pressure, levels of Basal excess and creatinine, and occurrence of arrhythmia, thus the clinician should evaluate the severity of methanol intoxication based on the history, lab results, vital signs and clinical symptoms in order to minimize morbidity and mortality.
Keywords: Alcoholism, Arrhythmias, Pressure, Cardiac Blood-
Creatinine, Disease Outbreaks, Ethanol, Iran, Methanol, Morbidity, Prognosis
Introduction
Methanol as a toxic alcohol has life threatening complications in poisoning, but with early referral and timely, correct, standard, and aggressive treatment, most of these complications could be prevented (1,2).
The Iranian Ministry of Health (MOH) and Legal Medicine Organization (LMO) recorded 5876 cases of methanol poisoning hospitalizations in the period of February 23, 2020 when the first COVID-19 case in Iran was documented until May 2, 2020. MOH reported 534 patients’ death with methanol poisoning in the hospital setting, which is equal to mortality rate of approximately 9% (534/5876). LMO registered 800 deaths from methanol poisoning during the same period, including both in-hospital and out-of-hospital fatalities (1).
Despite the prohibition of alcohol consumption in Islamic countries including Iran, there has been multiple methanol poisoning outbreaks in this country throughout the years for example, from September 7 to October 7, 2018, 768 people were registered as poisoned by methanol, of whom 76 died (10.1% fatality rate) (2) and in Rafsanjan province, between 29th May and 3rd June 2013, a total of 694 patients presented to emergency departments after public announcement of the outbreak and 8 patients expired due to the intoxication (3).
In 2018, in Malaysia, 31 patients presented with methanol poisoning which 19 patients died (61.3%) and out of those 12 patients who survived, 3 patients developed ophthalmologic complications (4). Between September 2016 and September 2019 in Turkey, 67 patients were registered as methanol poisoned patients which at the end 18 patients died (26.9%) and 14 patients (20.9%) discharged with central nervous system and visual sequelae (5).
Considering that the mean age of methanol poisoned patients were 32 years in Malaysia (4), 34.7±1.3years in Turkey (6), 21.5 years in Tunisia (7), it seems that this type of poisoning happens more in young people, but in Estonia, the age group between 50 and 60 years was most frequently represented (37%), and from 154 patients with methanol poisoning 68 patients (44%) died and 20 patients (13%) got discharged with permanent sequelae including impaired vision and brain damage (8).
In a study conducted in Taiwan, risk factors associated with mortality were low GCS (Glasgow Coma Scale), hypothermia and high creatinine levels (9). In another study conducted in Iran, GCS less than 8, pH less than 7.00 and inadequate hyperventilation were the risk factors for poor prognosis (10).
Due to higher prevalence of this problem in Iran, every time, especially during COVID-19 pandemic and its burden on health care system and its high mortality and morbidity, we conducted a study on patients with methanol poisoning in Tabriz, Iran. Understanding methanol poisoned patient’s socioeconomic status, the type of alcohol they consumed or the reason behind their alcohol consumption will help us to establish ways to prevent these incidences from happening, and discovering the potential risk factors will help physicians to make the right decisions regarding their treatment in a timely manner.
Materials and Methods
In this cross-sectional study, after obtaining the code of ethic IR.TBZMED.REC.144.092, the files of all the patients admitted to Tabriz Sina Hospital with complaint of methanol consumption or signs and symptoms associated with it from February 20th to June 20th, 2020 were investigated (inclusion criteria). The total number of cases was 224, but 40 cases were excluded due to concomitant poisoning with other drugs such as clonazepam, tramadol or bleach or consumption of other toxic alcohols including ethylene glycol, isopropyl alcohol or patients who refused the treatment and left the hospital against medical advice (exclusion criteria). The final number of samples was 184 and their demographic features, signs and symptoms , the amount of alcohol they consumed and intention of use, the time interval between alcohol consumption and the onset of the first symptom and the time interval between alcohol consumption and getting medical treatment, their vital signs upon arriving at the hospital, their laboratory findings and their outcome and permanent complications were collected and entered into SPSS (Statistical Package for Social Science software)(IBM Corp, Armonk, New York, USA) version 26 and were analyzed. All the lab data analyzed in this study were obtained at patient admission. Alpha error of 5% (95% confidence interval) was considered as the limit for rejecting or confirming a null hypothesis.
Results
A total of 184 patients were included in this study, 171 (92.93%) were male and 13 (7.06%) were female. Their mean age was 34.47±10.7 years, the minimum age was 15 years old and the maximum age was 65 years old 24.1% of the patients had some degree of college education, 72.2% had different levels of school education and 3.7% of the patients had no education at all. The most common type of alcohol that the methanol poisoned patients used was hand-made ethyl alcohol.
Alcohol types that Methanol poisoned patients ingested before admission to Sina Hospital in 63.4% of the patients were hand-made alcohol, in 26.9% of patients were industrial methyl alcohol and in 8.6% of patients were alcohol-based hand rubs.
Patients consumed alcohol for various reasons, files of 17 patients had no information about the reason behind alcohol consumption, 148 patients (80/4%) had alcohol use disorder and consumed alcohol as a leisure activity. 3 patients (1.6%) reported accidental and unintentional alcohol use and 12 patients (6.5%) reported alcohol consumption in order to prevent COVID19, 3 patients (1.6%) attempted suicide by drinking alcohol and one patient (0.0054%) reported that he was forced to drink alcohol as a criminal act.
The vital signs and level of consciousness at patient admission and before starting any medical treatment is listed in table 1. Among 184 patients, those who had low GCS levels, low SBP (systolic blood pressure), low MAP (mean arterial pressure) and low respiratory rate were prone to unfavorable outcomes. Patients’ pulse rate had no statistically significant effect on patients’ outcome.
The laboratory results in table 2 show that higher levels of creatinine, AST, ALT and PCO2 and lower levels of pH, BE and HCO3 are associated with higher morbidity and mortality.
Time interval between alcohol consumption and appearance of first symptom in two patients who died from methanol poisoning was 24.00±0 hr, but files of the rest of the patients (12 patients) who died did not have any data regarding this matter, in patients who survived methanol poisoning but had complications was 32.40±11.69 hr and in patients who survived methanol poisoning without any complications was 27.91±21.06 hr (p-value: 0.15).
Time interval between alcohol consumption and getting medical treatment in patients who died from methanol poisoning was 29.58±11.76 hr, in patients who survived methanol poisoning but had complications was 43.45±17.05 hr and in patients who survived methanol poisoning without any complications was 38.02±20.81 hr (p value: 0.1418).
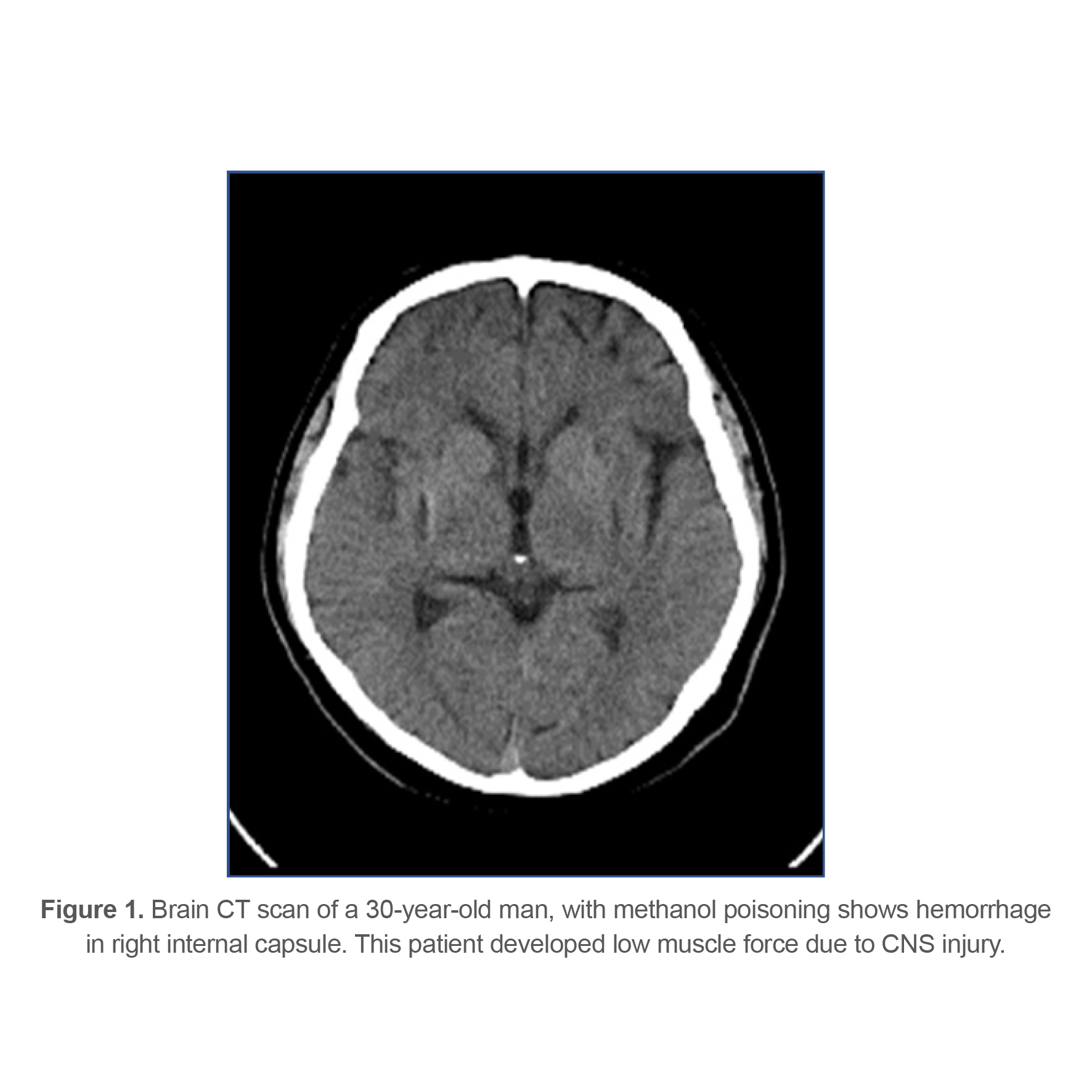
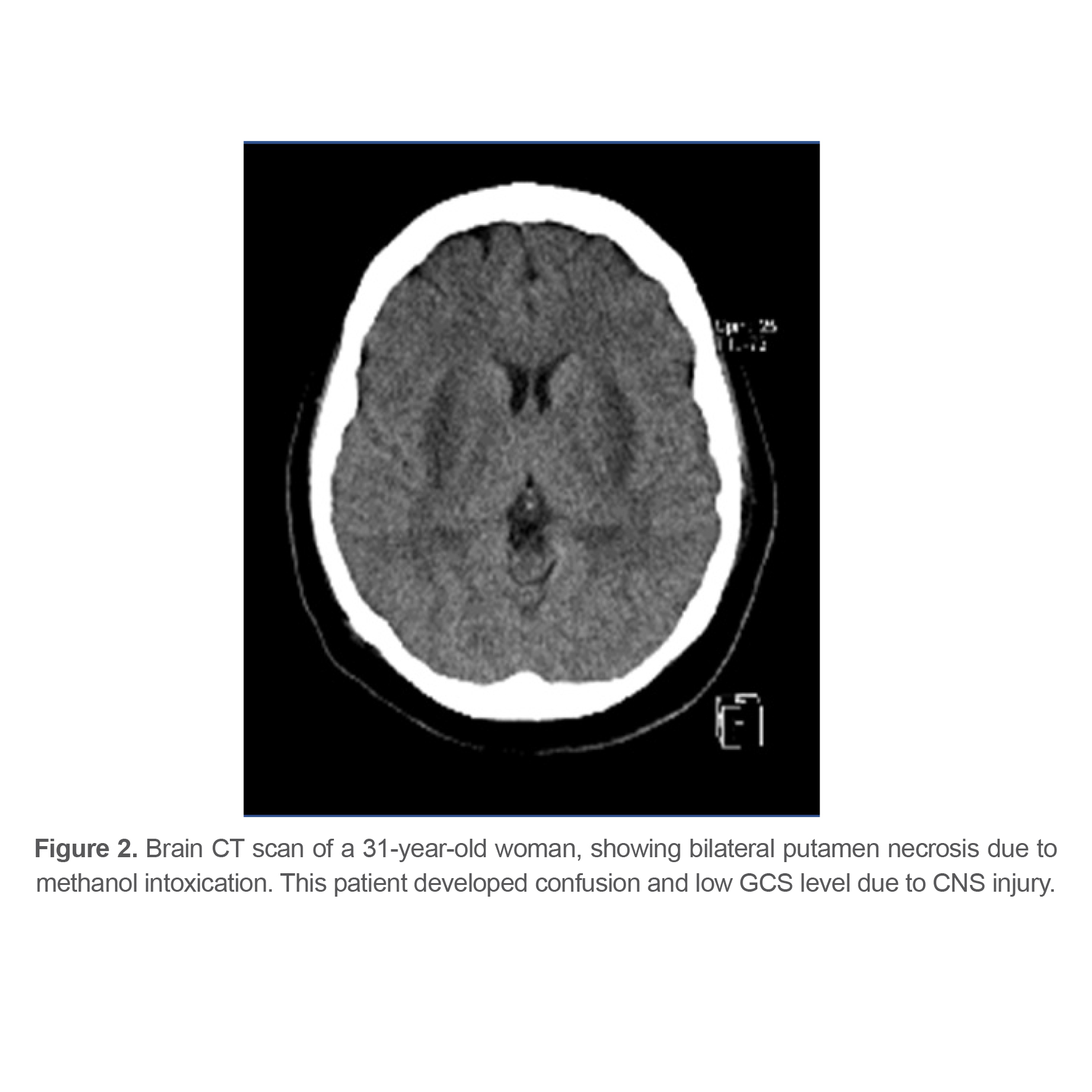
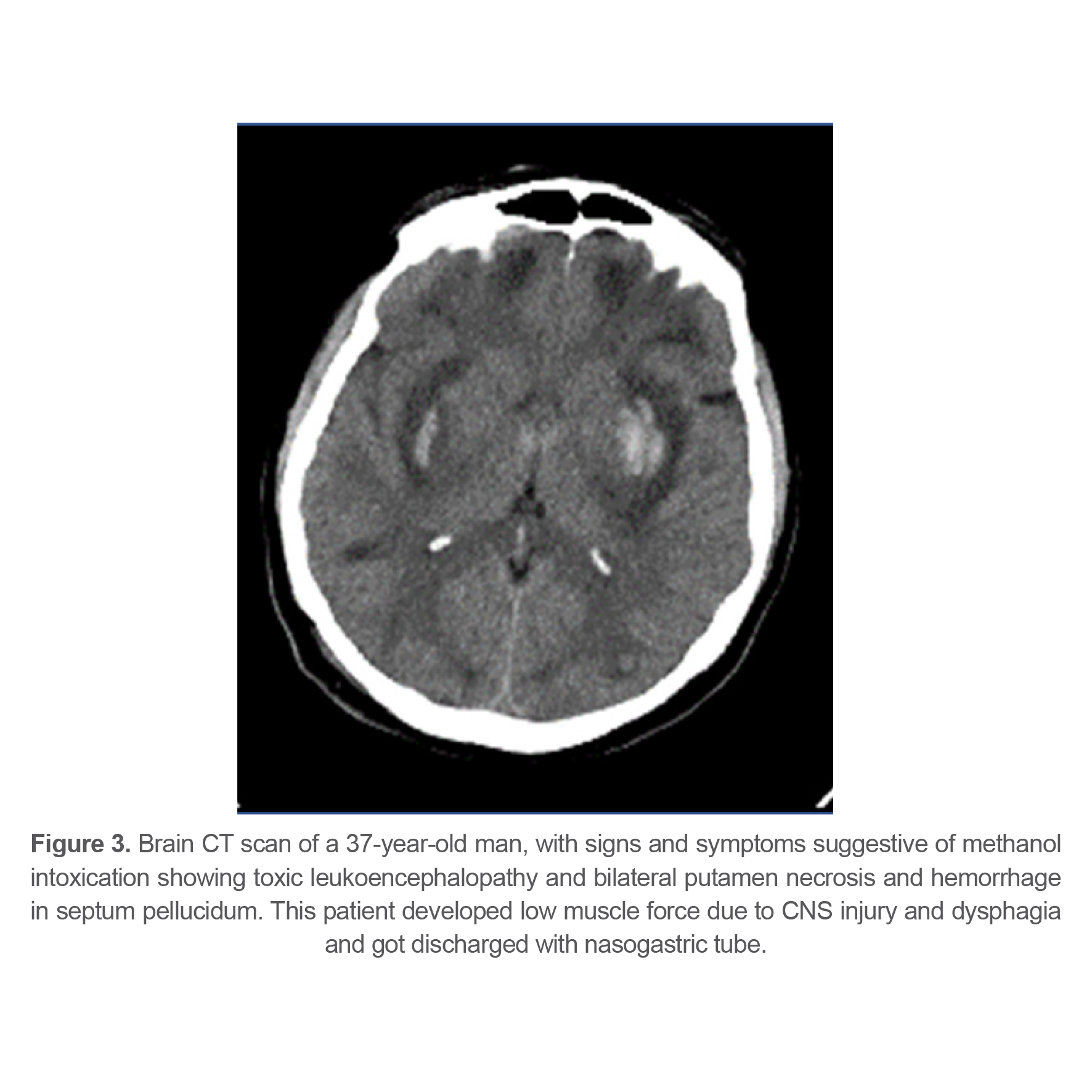
At last, 143 patients (77.72%) recovered completely, 27 patients (14.67%) had sequels at time of discharge from hospital and 14 patients (7.61%) died from methanol poisoning. Different types of complications and their frequency are listed in table 3. 21 patients (11.4%) had some sort of ophthalmologic complications at the time of discharge indicating that ophthalmologic complications were the most common complication among survivors. Figures 1-4 show brain CT scan of 4 patients with brain complications.
144 patients (78%) of 184 patients presented to the hospital with complaints of visual symptoms. At last, 114 of them (79.1%) survived completely, 24 of them (16.6%) survived but had complications and 6 of them (4.16%) died. 21 out of 24 patients who had sequels, developed different levels of visual impairment. Analysis showed that patients who presented to the hospital with complaints of visual symptoms are 0.82 less likely to die from methanol poisoning [OR (0.174) CI (0.056-0.536), p value= 0.002].
Two patients experienced seizures during hospitalization, one patient died and one patient survived without any complications; due to their limited number, analyzing the relationship between seizure and morbidity and mortality was not possible (p-value=0.072).
Three patients developed arrhythmia during hospitalization, two of them died and one of them survived but had complications. Analysis demonstrated that developing arrhythmia during hospitalization increases death possibility up to 28 times. [OR=28.16, CI 95% (2.38-333.27), p-value=0.008].
Table 1. Comparison of vital signs of the patients upon arrival at the hospital in methanol-poisoned patients admitted in Sina Hospital
|
|
Full recovery (Mean±SD) |
Partial recovery (Mean±SD) |
Death (Mean±SD) |
p-value |
|
GCS |
14.21±1.98 |
11.76±4.35 |
5.33±2.34 |
<0.001 |
|
SBP |
123.69±21.50 |
114.96±16.23 |
103.14±48.67 |
0.004 |
|
MAP |
92.07±16.69 |
85.69±11.41 |
72.28±36.53 |
<0.001 |
|
Pulse rate |
99.83±87.59 |
97.11±18.24 |
82.07±37.22 |
0.738 |
|
Respiratory rate |
18.89±4.42 |
19.43±5.03 |
11.00±9.84 |
<0.001 |
Table 2. Comparison of laboratory results at patients’ admission in methanol-poisoned patients
|
Laboratory findings |
Full recovery (Mean±SD) |
Partial recovery (Mean±SD) |
Death (Mean±SD) |
p-value |
|
WBC |
11223.3±6861.3 |
14576.1±6050.1 |
13223.0±5871.7 |
0.050 |
|
Hemoglobin |
17.14±2.65 |
16.53±3.04 |
15.33±2.35 |
0.055 |
|
Hematocrit |
49.88±6.55 |
49.55±7.55 |
46.73±7.97 |
0.284 |
|
Platelet×103 |
242.76±68.87 |
277.34±103.94 |
228.15±71.15 |
0.067 |
|
Blood Sugar |
127.94±54.68 |
131.76±50.20 |
140.30±54.29 |
0.713 |
|
Urea |
26.58±10.12 |
31.33±11.51 |
24.69±8.70 |
0.061 |
|
Creatinine |
1.24±0.39 |
1.48±0.47 |
1.67±0.55 |
< 0.001 |
|
AST |
35.60±47.01 |
49.46±83.77 |
189.91±123.99 |
< 0.001 |
|
ALT |
35.13±32.19 |
52.61±100.19 |
101.83±71.22 |
< 0.001 |
|
ALK P |
230.88±89.00 |
245.28±106.95 |
279.16±155.81 |
0.259 |
|
Potassium |
4.62±0.77 |
4.44±0.86 |
4.47±1.30 |
0.543 |
|
Sodium |
139.95±10.92 |
139.65±2.66 |
144.5±5.17 |
0.296 |
|
Magnesium |
2.23±0.66 |
2.15±0.48 |
1.56±0.32 |
0.129 |
|
Calcium Ion |
1.02±0.16 |
1.02±0.05 |
1.12±0.16 |
0.445 |
|
Calcium Total |
8.14±2.41 |
7.84±0.44 |
7.62±1.02 |
0.825 |
|
pH |
7.17±0.10 |
7.05±0.18 |
6.77±0.14 |
< 0.001 |
|
Basal Excess |
-16.83±6.48 |
-22.17±5.33 |
-27.69±4.80 |
< 0.001 |
|
PCO2 |
25.06±9.19 |
25.51±12.51 |
53.84±19.22 |
< 0.001 |
|
HCO3 |
9.95±5.30 |
6.60±2.25 |
8.03±3.28 |
0.004 |
|
CPK |
521.0±1293.3 |
1978.0±4450.5 |
1407.2±1835.7 |
0.164 |
|
LDH |
510.5±264.9 |
585.6±94.0 |
406.0±0.0 |
0.798 |
Table 3. Permanent impairment and complications of methanol toxicity during discharge in Methanol-poisoned patients admitted in Sina Hospital
|
|
Frequency |
Percentage |
|
Dysphagia and needing nasogastric tube |
3 |
1.6 |
|
Acute kidney injury *1 |
1 |
0.5 |
|
Dysphasia |
1 |
0.5 |
|
Tracheostomy *2 |
2 |
1.1 |
|
Decreased muscle force due to CNS injury |
6 |
3.2 |
|
Complete vision loss (no light perception) |
2 |
1.1 |
|
Vision impairment (counting fingers) |
4 |
2.2 |
|
Vision impairment (light perception) |
2 |
1.1 |
|
Blurred vision |
13 |
7 |
|
Cognitive deficit *3 |
3 |
1.6 |
*1. One of the patients continued to have high creatinine level upon discharge and was diagnosed with acute kidney injury.
*2. Two patients went through tracheostomy procedure and were referred to pulmonology clinic for possible bronchoscopy and deciding about its removal.
*3. Three patients developed cognitive deficit and based on neurology consultation needed medical treatment and follow-up with neurology department.
Discussion
In COVID-19 pandemic, there was more focus on preventing and controlling this disease, but a challenging problem which arose in Iran that time was methanol poisoning which resulted in additional workload on hospital staff and complications in patients (1).
In this study, 171 patients (92.9%) were male and 13 patients (7.06%) were female. In another study performed in Isfahan-Iran between 2000-9, 84.3% of the patients were male and 15.7% were female (11). In Malaysia, in 2018, 30 patients out of 31 methanol-poisoned patients were male (4). We speculate that this might be due to fact that men have more access to hand-made alcohol or industrial alcohol and alcohol addiction is more common among men than women, thereby methanol poisoning due to non-standard ethyl alcohol misuse occurs more often in men.
In this study, 27 patients (14.67%) had complications upon discharge from the hospital and 14 patients (7.61%) died from methanol poisoning, in a methanol poisoning epidemic in Estonia from 154 patients, 68 patients (44%) died and 20 patients developed complications including visual impairment and brain injury (8). The reason behind the fact that a popular explanation of lower morbidity and mortality in Tabriz-Sina Hospital is that comparing to other centers methanol poisoning is fairly prevalent in Iran and medical staff are competent in diagnosing and treating this condition and dialysis which is a crucial part of the treatment readily available.
This study showed that visual symptoms on admission has protective effects against morbidity and mortality. This could be due to the fact that patients who developed vision impairment were more likely to go to the hospital in comparison to patients who had non-specific signs and symptoms. Alternatively, it could simply mean that patients who first presented to the hospital with low GCS and eventually died were unable to give a thorough history and mention vision impairment.
In line with recent studies, low respiratory rate, SBP, MAP and GCS upon arrival at the hospital and abnormal blood tests including increased levels of creatinine, PCO2, AST and ALT and decreased levels of pH and BE were associated with unfavorable outcomes; in a study in Czech Republic in 2012, pH lower than 7, negative ethanol serum and coma upon arrival at the hospital were independent parameters in anticipating death due to methanol poisoning (12). In Taiwan low GCS, hypothermia and raised creatinine were associated with morbidity and mortality (9). In Nigeria (13), delayed hospital presentation was related to bad outcomes, but in this study, there was no association between time interval between alcohol consumption and starting the treatment which is a result of insufficient data in this field.
Research limitations: a major limitation in this study is that some patients were at first admitted in other hospitals and then got transferred to Sina Hospital, their vital signs or laboratory results before any treatments were not available and the file records of some patients did not have all the needed information for this study. Another limitation was some patients who were admitted to the hospital with loss of consciousness and eventually died were unable to give a thorough history about visual impairment or other signs.
Conclusion
According to this study, the clinician should evaluate the severity of methanol intoxication based on the history, lab results, vital signs and clinical symptoms in order to minimize permanent complications and mortality through proper and timely interventions. In our study, in-hospital cardiac arrhythmia rises mortality to 28 times greater, and poor outcome was associated with low respiratory rate, SBP, MBP, or GCS upon arrival at the hospital and lab results analysis showed that elevated levels of creatinine, AST, ALT, or PCO2 and decreased levels of pH, or HCO3 were best predictors of morbidity and mortality. Our results demonstrated that patients who expressed vision problems were less likely to die or end up with complications.
Declarations
Ethics approval and consent to participate
All the methods were carried out in accordance with relevant guidelines and regulations. Ethical clearance was obtained from the Regional Ethics Committee (Research Ethics Committees of Tabriz University of Medical Sciences; Approval ID (code): IR.TBZMED.REC.144.092). Also, during hospitalization, informed consent was obtained from all the subjects and/or their legal guardian (s) for human data use; and the patients’ information remained confidential in this study. Ethical clearance for beginning this research and publication of results was obtained from the Research Ethics Committee of Tabriz University of Medical Sciences: IR.TBZMED.REC.144.092; and based on this clearance Consent for Publication is missing in the manuscript.
Consent for Publication
Not Applicable as no identifying data/information is present in the manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, private, or not-for-profit sectors.